Embryo Grading and Selection in IVF
One of the most important steps in the IVF process happens in the lab, far away from what patients can see. After fertilization, the embryo begins to grow and develop. At this stage, embryologists use grading systems to decide which embryos have the best potential for implantation and pregnancy. For many patients, embryo grading can feel like a mystery, yet it plays a significant role in IVF success. (Source: MDPI)
What Embryo Grading Means
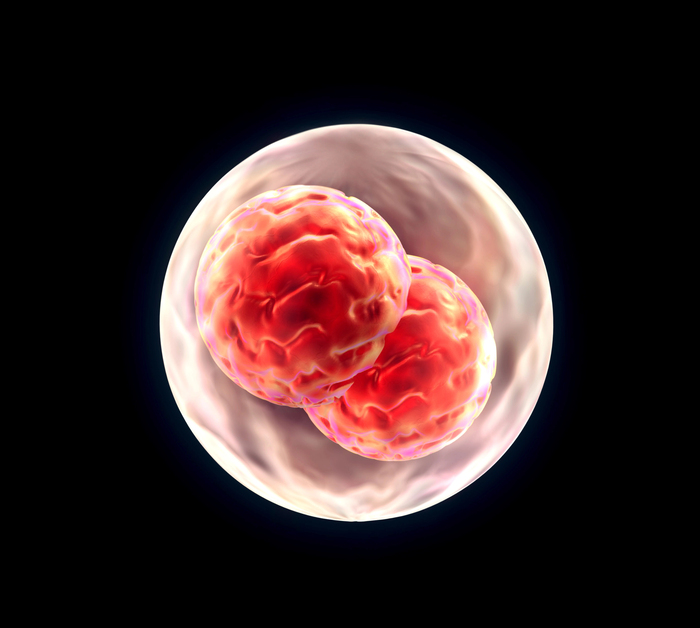
Embryo grading is a way to measure how healthy an embryo looks under a microscope. Embryologists look at things like the number of cells, how evenly the cells divide, and whether the embryo shows signs of normal development. Grading does not reveal everything about an embryo’s genetic health, but it provides valuable information about which embryos are most likely to result in a successful pregnancy.
In the early stages, embryos are typically assessed on day three, when they consist of just a few cells. At this point, doctors look for embryos that have the right number of cells for their age and that divide in a balanced way. Later, on day five or six, embryos reach what is called the blastocyst stage. At this stage, grading focuses on how well the inner cell mass and the outer layer of cells are forming. These two parts are critical because the inner mass becomes the fetus, and the outer layer develops into the placenta.
Why Embryo Selection Matters
IVF often produces several embryos, but not all of them will continue to grow normally. Some may stop dividing, while others may show uneven cell development. By using grading systems, embryologists can select the embryos with the highest chance of implanting successfully in the uterus.
Embryo selection is especially important when deciding how many embryos to transfer. The goal in most clinics today is to transfer a single high-quality embryo to reduce the risk of multiple pregnancies while keeping success rates high. Knowing which embryo has the best potential helps doctors make safer and more effective decisions. (Source: PubMed)
The Limits of Grading
While grading is useful, it is not a guarantee of success. An embryo with a high grade can still fail to implant, while a lower-grade embryo may still lead to a healthy pregnancy. This is because grading only looks at appearance, not genetic health. Chromosomal problems, which are one of the leading causes of failed implantation or miscarriage, cannot be detected by grading alone.
To get more accurate information, some patients choose to combine embryo grading with genetic testing methods such as preimplantation genetic testing (PGT). PGT can identify chromosomal abnormalities that grading cannot detect, providing an even clearer picture of embryo health. (Source: Science Direct)
What Patients Should Know
For patients, hearing about embryo grades can feel overwhelming. It is natural to worry when an embryo is not graded as “perfect.” But it is important to remember that many healthy babies have been born from embryos that were not top-graded in the lab. Grading is just one tool among many that doctors use to increase the chances of success.
What matters most is that the selection process gives patients the best possible chance with each transfer. Behind every grade and every decision is a careful effort by embryologists and doctors to make IVF treatment as effective and safe as possible.
Sources:
MDPI - MDPI.com/2077-0383/13/2/626
PubMed - PubMed.ncbi.nlm.nih.gov/34819249/
Science Direct - https://www.sciencedirect.com/science/article/abs/pii/S001502822500216X